As the healthcare industry continues its digital transformation, it’s important to remember the breakthroughs that lead us to where we are today. Whether in medical technology or medicine itself, advances in how care is delivered to patients rest on the shoulders of medical pioneers.
When Andreas Roland Grüntzig, a German radiologist and cardiologist, developed interventional cardiology, the medical world was astonished. For the first time, someone had found a way to treat cardiovascular disease using only a catheter, thus avoiding open heart surgery.
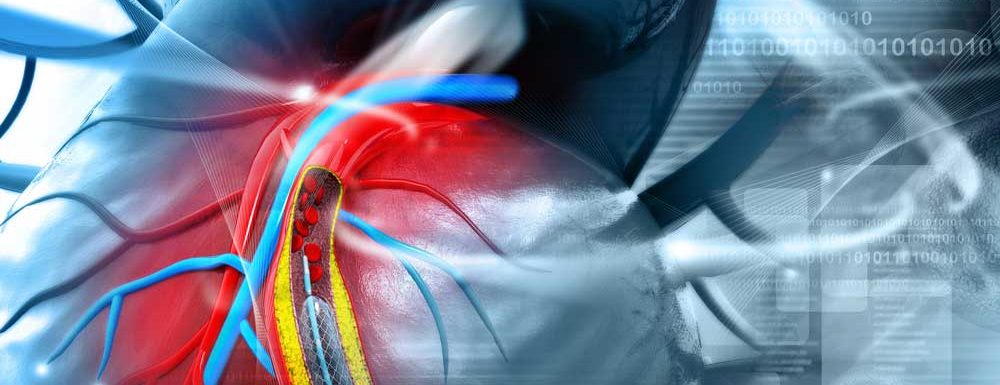
Nowadays, physicians around the globe perform catheter-based procedures such as angioplasty and stenting to treat heart arteries clogged by plaque.Thanks to X-rays, MRIs and other advanced technologies used by interventional cardiologists, patients recover faster, have no scars and experience less pain.
Here are some points worth knowing about these complex and fascinating medical procedures:
- There are more coronary angioplasties performed annually than coronary bypass operations.
Coronary artery disease (CAD) is caused by the buildup of plaque or fatty deposits inside of the heart’s arterial walls. When arteries get clogged, less blood is pumped to the heart, which can cause a heart attack. CAD is the leading cause of death in the United States in both men and women.
For a long time, coronary bypass surgery (open heart surgery) was the most common way to treat CAD. Open heart surgery, though, is hard on the body and carries many risks. Not only can it lead to complications such as infections and kidney failure, but it also leaves distinctive scars and recovery can take up to six months.
This procedure has increasingly been replaced by coronary angioplasties. First performed in the United States by Dr. Simon Stertzer in 1978, coronary angioplasties are far less invasive and often more effective than a bypass. During an angioplasty, a small balloon-tipped stent is inserted through an artery in the groin or wrist to enlarge a narrowing coronary artery and restore blood flow. Patients can go home the same day, without scars or complications. Each year, about 600,000 people in the United States undergo angioplasty surgery, versus 400,000 who have a bypass.
- Aortic, mitral and even tricuspid cardiac valves can be treated from the outside of the body, without open heart surgery.
The heart has four valves that control blood flow into the heart’s chambers. When one of those doesn’t work properly, people develop heart valve disease, which can cause heart failure, stroke, blood clots or sudden death. To treat it, doctors used to recommend open heart surgery. Interventional cardiology made it possible for heart valves to be repaired with catheters, from outside of the body.
During this procedure, a doctor uses a catheter to insert clips and other devices into a patient’s blood vessels to reshape the valve and restore blood flow. In some cases, the valve needs to be completely replaced with one made from cow or pig heart tissue. This procedure is called transcatheter aortic valve replacement (TAVR).
Watch this video to see how it’s done without having to open the chest cavity.
- Metal and drug delivery stents now drastically reduce the need for repeat angioplasty.
In interventional cardiology, stents can do much more than restore blood flow after angioplasty. It’s not uncommon for a patient’s arteries to again become clogged after a procedure. This time, the clog is caused not by fatty deposits, but by excess tissue. The effect is similar to a scar forming over an injury.
This phenomenon, called restenosis, could once only be reversed by repeating the angioplasty. Innovative drug-eluting stents (DES) changed that. These stents are coated in polymer, a material that carries and controls the release of drugs to coronary and peripheral arteries, keeping the blockage from reforming. Using DES, the blockage vanishes without leaving any traces. New generation drug-eluting stents have significantly reduced in-stent restenosis.
- Implantable defibrillators reduce the incidence of sudden death in carefully selected patients.
Sudden cardiac death (SCD) is among the most common causes of death in the United States. According to the Centers for Disease Control and Prevention, there are an estimated 356,000 SCDs per year. A history of previous heart attacks and coronary artery disease often accompany SCD.
Usually, SCDs occur in patients with heart abnormalities; their hearts simply stop functioning, without any previously diagnosed fatal condition.
Nowadays, implantable defibrillators can quickly detect and treat life‐threatening arrhythmias (abnormal heart rhythm).
Unlike current subcutaneous defibrillators, implantable ones replace the metal pulse generator pocket with a single flexible, string-shaped device with no leads within the heart. They are especially valuable for groups with a higher risk of SCD, such as young athletes or people on dialysis. Some devices, such as the ISSD designed by Newpace, can be connected to a smartphone.
- Trials in which stem cells are implanted into failing heart muscles are currently underway.
Heart failure occurs when the heart is not able to pump enough blood throughout the body, particularly after it has been weakened by a heart attack. Recent estimates show that over 131 million adults will have experienced heart failure in the United States by 2035.
Researchers are working to solve this problem with the help of stem cells.
Biocardia, for example, is a clinical-stage regenerative biotechnology company that develops novel therapeutics to treat heart disease. Its therapies use cell regeneration to treat heart failure after a heart attack. In one investigational therapy, the only items required are the patient’s own cells, which are separated from the bone marrow plasma and injected into the affected areas of the heart using a catheter. The entire procedure lasts between 60 and 90 minutes, and the patient returns home the same day.
Leave a Reply